Battling Foot Problems From Diabetes

Diabetes can have a profound impact on foot health, leading to complications such as nerve damage and poor circulation. These issues increase the risk of developing sores, infections, and even severe conditions that may necessitate amputation. Daily foot checks are essential for early detection of cuts, blisters, or signs of infection. Wearing appropriate socks is also important. Choose socks that wick away moisture, fit well, and are free of seams to prevent irritation. Selecting the right footwear is also important. Ensure that your shoes fit well, but also leave some room for toe movement to avoid pressure points. It's also advisable to avoid walking barefoot, even indoors, to protect against unnoticed injuries. Diabetic patients with venous insufficiency or swelling may benefit from wearing compression socks but should consult their podiatrist for the best options. Good foot hygiene, including washing with warm water and drying thoroughly, helps prevent fungal infections. Keeping toenails trimmed straight across can prevent ingrown toenails, which are another potential source of infection. Regular visits to a podiatrist can help manage and monitor foot health, preventing minor issues from escalating. If you experience diabetic foot pain, it is suggested that you schedule an appointment with a podiatrist for an exam and treatment options.
Diabetic foot care is important in preventing foot ailments such as ulcers. If you are suffering from diabetes or have any other concerns about your feet, contact Naim G. Shaheed, DPM from Ankle and Foot Centers of Georgia. Our doctor can provide the care you need to keep you pain-free and on your feet.
Diabetic Foot Care
Diabetes affects millions of people every year. The condition can damage blood vessels in many parts of the body, especially the feet. Because of this, taking care of your feet is essential if you have diabetes, and having a podiatrist help monitor your foot health is highly recommended.
The Importance of Caring for Your Feet
- Routinely inspect your feet for bruises or sores.
- Wear socks that fit your feet comfortably.
- Wear comfortable shoes that provide adequate support.
Patients with diabetes should have their doctor monitor their blood levels, as blood sugar levels play such a huge role in diabetic care. Monitoring these levels on a regular basis is highly advised.
It is always best to inform your healthcare professional of any concerns you may have regarding your feet, especially for diabetic patients. Early treatment and routine foot examinations are keys to maintaining proper health, especially because severe complications can arise if proper treatment is not applied.
If you have any questions please feel free to contact one of our offices located in Lithonia/Stonecrest and Emory/Midtown, GA . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
How to Care for Diabetic Foot
Millions of people are affected by diabetes each year. Diabetes damages blood vessels in all parts of the body, especially the feet. The legs and feet may develop slow blood flow, which causes neuropathy, or nerve damage. Once a diabetic patient develops neuropathy, it is important that the feet are well taken care of. Otherwise, the lower limbs may have to be amputated. This only happens in drastic cases, but it shows how seriously diabetic foot care should be taken.
It is very important to always wash and dry the feet thoroughly, especially in between the toes, if you’re a diabetic. Secondly, examining your feet and toes for redness or sores must be done, even if you do not feel pain. You may also want to examine your feet from the bottom. Try to avoid wearing colored socks to prevent infections that may occur from the dye. Well-fitting socks are also highly recommended.
A diabetic’s physician should always monitor their blood levels to test how well blood sugars are being maintained. In addition to giving advice about everyday eating habits and foot care, a physician may prescribe medicine to help with the diabetic patient’s neuropathy. It is also advised to see a podiatrist if experiencing any feet conditions. Toenails may also need to be taken care of by a podiatrist. This prevents patients from cutting too deeply around their cuticles, which can lead to infection.
A person can take care of their feet at home by following the instructions of their physician. Using creams on one’s feet is also an effective way to heal dryness. Proceed with caution when using tools to remove calluses, as severe diabetics may not be able to feel pain on their feet. If any complications arise do not hesitate to contact a podiatrist.
On a daily basis, diabetic feet must be checked. If you are ever concerned about something, contact your health care professional. You never want to wait until a wound becomes too severe to treat. If left untreated, gangrene may develop. Gangrene is a serious infection that can lead to sepsis or amputation. It is also important for diabetics to be on the lookout for ulcers. Ulcers are sores that develop from tissue loss on the skin. They can be quite painful and require intensive treatment. Early treatment and everyday inspection are imperative to staying healthy.
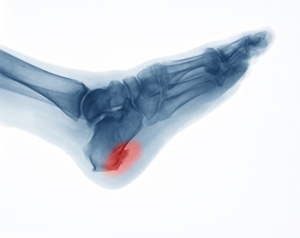
Causes and Definition of Heel Spurs
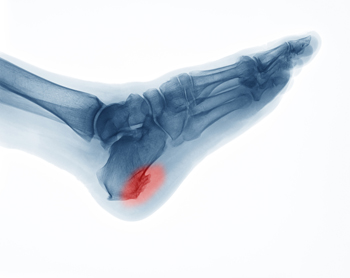 A heel spur, medically known as a calcaneal spur, is a bony growth that develops on the underside of the heel bone. This condition often results from long-term strain on the foot muscles and ligaments, commonly associated with repetitive activities such as running or jumping. Over time, this strain leads to the accumulation of calcium deposits, forming the bony protrusion. Heel spurs are frequently linked to plantar fasciitis, an inflammation of the plantar fascia tissue that runs along the bottom of the foot. Factors contributing to heel spur development include wearing ill-fitting shoes, excessive weight, and having flat feet or high arches. If you have heel pain, it may be indicative of a heel spur, and it is suggested that you consult a podiatrist who can accurately diagnose and offer a comprehensive treatment plan for heel spurs.
A heel spur, medically known as a calcaneal spur, is a bony growth that develops on the underside of the heel bone. This condition often results from long-term strain on the foot muscles and ligaments, commonly associated with repetitive activities such as running or jumping. Over time, this strain leads to the accumulation of calcium deposits, forming the bony protrusion. Heel spurs are frequently linked to plantar fasciitis, an inflammation of the plantar fascia tissue that runs along the bottom of the foot. Factors contributing to heel spur development include wearing ill-fitting shoes, excessive weight, and having flat feet or high arches. If you have heel pain, it may be indicative of a heel spur, and it is suggested that you consult a podiatrist who can accurately diagnose and offer a comprehensive treatment plan for heel spurs.
Heel spurs can be incredibly painful and sometimes may make you unable to participate in physical activities. To get medical care for your heel spurs, contact Naim G. Shaheed, DPM from Ankle and Foot Centers of Georgia. Our doctor will do everything possible to treat your condition.
Heels Spurs
Heel spurs are formed by calcium deposits on the back of the foot where the heel is. This can also be caused by small fragments of bone breaking off one section of the foot, attaching onto the back of the foot. Heel spurs can also be bone growth on the back of the foot and may grow in the direction of the arch of the foot.
Older individuals usually suffer from heel spurs and pain sometimes intensifies with age. One of the main condition's spurs are related to is plantar fasciitis.
Pain
The pain associated with spurs is often because of weight placed on the feet. When someone is walking, their entire weight is concentrated on the feet. Bone spurs then have the tendency to affect other bones and tissues around the foot. As the pain continues, the feet will become tender and sensitive over time.
Treatments
There are many ways to treat heel spurs. If one is suffering from heel spurs in conjunction with pain, there are several methods for healing. Medication, surgery, and herbal care are some options.
If you have any questions feel free to contact one of our offices located in Lithonia/Stonecrest and Emory/Midtown, GA . We offer the latest in diagnostic and treatment technology to meet your needs.
Heel Spurs
Heel spurs are the result of calcium deposits that cause bony protrusions on the underside of the heel. Heel spurs are usually painless, but they have the potential to cause heel pain. Heel spurs tend to be associated with plantar fasciitis, which is a condition that causes inflammation of the band of connective tissue that runs along the bottom of the foot. They most often occur to athletes whose sports involve a lot of running and jumping.
Some risk factors for developing heel spurs include running and jogging on hard surfaces, being obese, wearing poorly fitting shoes, or having walking gait abnormalities.
It is possible to have a heel spur without showing signs of any symptoms. However, if inflammation develops at the point of the spur’s formation, you may have pain while walking or running. In terms of diagnosis, sometimes all a doctor needs to know is that the patient is experiencing a sharp pain localized to the heel to diagnose a heel spur. Other times, an x-ray may be needed to confirm the presence of a heel spur.
Heel spurs can be prevented by wearing well-fitting shoes that have shock-absorbent soles. You should also be sure that you are choosing the right shoe for the activity you want to partake in; for example, do not wear walking shoes when you want to go on a run. Additionally, maintaining a healthy weight can be beneficial toward preventing heel spurs, as it will prevent an excess amount of pressure being placed on the ligaments.
There are a variety of treatment options for people with heel spurs. Some of these include stretching exercises, physical therapy, shoe inserts, or taping and strapping to rest stressed muscles and tendons. If you have heel pain that lasts longer than a month, don’t hesitate to seek help from a podiatrist. Your doctor can help you determine which treatment option is best for you.
Effective and Easy Exercises for Plantar Fasciitis Relief

Relieving plantar fasciitis pain can be achieved through simple exercises that stretch and strengthen the foot. One effective exercise is the calf stretch, where you lean against a wall with one leg extended back and the other bent forward, stretching the calf muscles and reducing tension on the plantar fascia. The toe stretch involves sitting down and pulling your toes back toward your shin, helping to loosen the fascia. Rolling a tennis ball or frozen water bottle under your foot can massage and alleviate pain. Performing foot flexes by sitting with your legs straight and using a towel to pull your toes toward you can also provide relief. Consistently practicing these exercises can reduce pain and inflammation, promoting healing and preventing future flare-ups. If you have plantar fasciitis and are seeking additional effective foot stretches for relief, it is suggested that you visit a podiatrist, who can provide you with the information you are seeking.
Plantar fasciitis can be very painful and inconvenient. If you are experiencing heel pain or symptoms of plantar fasciitis, contact Naim G. Shaheed, DPM from Ankle and Foot Centers of Georgia. Our doctor can provide the care you need to keep you pain-free and on your feet.
What Is Plantar Fasciitis?
Plantar fasciitis is the inflammation of the thick band of tissue that runs along the bottom of your foot, known as the plantar fascia, and causes mild to severe heel pain.
What Causes Plantar Fasciitis?
- Excessive running
- Non-supportive shoes
- Overpronation
- Repeated stretching and tearing of the plantar fascia
How Can It Be Treated?
- Conservative measures – anti-inflammatories, ice packs, stretching exercises, physical therapy, orthotic devices
- Shockwave therapy – sound waves are sent to the affected area to facilitate healing and are usually used for chronic cases of plantar fasciitis
- Surgery – usually only used as a last resort when all else fails. The plantar fascia can be surgically detached from the heel
While very treatable, plantar fasciitis is definitely not something that should be ignored. Especially in severe cases, speaking to your doctor right away is highly recommended to avoid complications and severe heel pain. Your podiatrist can work with you to provide the appropriate treatment options tailored to your condition.
If you have any questions please feel free to contact one of our offices located in Lithonia/Stonecrest and Emory/Midtown, GA . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
Plantar Fasciitis
The plantar fascia is a connective tissue in the heel that stretches across the bottom length of your foot. Plantar fasciitis occurs when the connective tissue becomes inflamed, causing heel pain and discomfort during physical activity. Although the condition is completely treatable, traditional methods can take up to a year to start becoming effective.
Plantar fasciitis is caused by a number of everyday activities, so understanding the condition is important for managing and treating it. One of the most common causes of plantar fasciitis is excessive running, especially with improper fitting or non-supportive shoes. Too much exercise can lead to the plantar fascia being overworked and overstretched, which can cause tears in the tissue. Along with improper fitting shoes, pronation, the rolling of the feet inward, is a common cause of plantar fasciitis. If not treated properly, the plantar fascia becomes overstretched and starts to tear, causing inflammation.
Despite the common causes of plantar fasciitis, there are many different treatment options. For less severe cases, conservative home remedies include taking anti-inflammatory drugs to alleviate pain, applying ice packs to the bottom of your foot and heel, slowly stretching and exercising your feet to re-strengthen the tissue, and using orthotic devices are all ways to help manage your plantar fasciitis.
For more severe cases, shockwave therapy has become a common solution for plantar fasciitis. Shockwave therapy can effectively break up the tissue on the bottom of your foot which facilitates healing and regeneration. This fights the chronic pain caused by plantar fasciitis. Even if this doesn’t work, surgery is always a final option. Surgery on the tissue itself can be done to permanently correct the issue and stop the inflammation and pain in your heels.
No matter what the case may be, consulting your podiatrist is the first and best step to recovery. Even the slightest amount of heel pain could be the first stage of plantar fasciitis. Untreated symptoms can lead to the tearing and overstretching of tissue. Because the tearing of tissue can be compounded if it remains ignored, it can evolve into a severe case. The solution is early detection and early treatment. Talk to your podiatrist about the possibilities of plantar fasciitis if you’re experiencing heel pain.
Diagnosis and Symptoms of Foot Puncture Wounds

Foot puncture wounds are injuries where a sharp object pierces the skin and underlying tissues of the foot. These wounds can occur from stepping on nails, glass, or other sharp objects. Proper diagnosis involves a physical examination by a podiatrist, often accompanied by imaging tests like X-rays to assess the depth and presence of foreign objects. Symptoms of a foot puncture wound include pain, swelling, redness, and bleeding at the site of injury. If the wound becomes infected, additional symptoms such as warmth, pus, and increased pain may develop. Timely medical attention is vital to clean the wound thoroughly, prevent infection, and ensure proper healing. If you have stepped on a sharp object and have developed a foot wound, it is suggested that you seek prompt medical treatment from a podiatrist who can effectively manage this condition.
Wound care is an important part in dealing with diabetes. If you have diabetes and a foot wound or would like more information about wound care for diabetics, consult with Naim G. Shaheed, DPM from Ankle and Foot Centers of Georgia. Our doctor will assess your condition and provide you with quality foot and ankle treatment.
What Is Wound Care?
Wound care is the practice of taking proper care of a wound. This can range from the smallest to the largest of wounds. While everyone can benefit from proper wound care, it is much more important for diabetics. Diabetics often suffer from poor blood circulation which causes wounds to heal much slower than they would in a non-diabetic.
What Is the Importance of Wound Care?
While it may not seem apparent with small ulcers on the foot, for diabetics, any size ulcer can become infected. Diabetics often also suffer from neuropathy, or nerve loss. This means they might not even feel when they have an ulcer on their foot. If the wound becomes severely infected, amputation may be necessary. Therefore, it is of the upmost importance to properly care for any and all foot wounds.
How to Care for Wounds
The best way to care for foot wounds is to prevent them. For diabetics, this means daily inspections of the feet for any signs of abnormalities or ulcers. It is also recommended to see a podiatrist several times a year for a foot inspection. If you do have an ulcer, run the wound under water to clear dirt from the wound; then apply antibiotic ointment to the wound and cover with a bandage. Bandages should be changed daily and keeping pressure off the wound is smart. It is advised to see a podiatrist, who can keep an eye on it.
If you have any questions, please feel free to contact one of our offices located in Lithonia/Stonecrest and Emory/Midtown, GA . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Wound Care
Diabetics must be wary of all wounds, regardless of depth or size. Diabetes, a chronic disease in which the body cannot properly use glucose the way it normally would, causes various complications that make wounds difficult to heal. Nerve damage or neuropathy will cause diabetics to have trouble feeling the pain of a blister or cut until the condition has significantly worsened or become infected. A diabetic’s weakened immune system can make even the most minor of wounds easily susceptible to infection. Diabetics are also more prone to developing narrow, clogged arteries, and are therefore more likely to develop wounds.
Wounds should be taken care of immediately after discovery, as even the smallest of wounds can become infected if enough bacteria build up within the wound. To remove dirt, wounds should be first rinsed under running water only. Soap, hydrogen peroxide, or iodine can irritate the injury and should be avoided. To prevent infection, apply antibiotic ointment to the wound and cover it with a bandage. The bandage should be changed daily. The skin around the wound may be cleaned with soap.
To prevent further exacerbation, see a doctor—especially if you have diabetes. Minor skin conditions can become larger problems if not properly inspected. As the wound heals, make sure to avoid applying pressure to the affected area.
Possible Complications of a Broken Ankle

A broken ankle, medically termed ankle fracture, poses significant risks and complications, particularly for active individuals and the elderly. Active individuals are often at risk due to participation in high-impact activities, while the elderly are susceptible due to factors such as decreased bone density and balance issues. One potential complication of a broken ankle is the development of osteoarthritis in the affected joint over time. This occurs due to the disruption of the joint's normal structure and function during the healing process, leading to cartilage degeneration and subsequent pain and stiffness. Elderly individuals, especially those with diabetes, are also prone to complications such as wound healing issues and infections, which can prolong recovery and increase the risk of further complications. Treatment for a broken ankle typically involves immobilization with a cast or brace and pain management. If you have sustained an ankle fracture, it is suggested that you schedule an appointment with a podiatrist who can provide comprehensive care, including monitoring for complications, optimizing rehabilitation, and providing long-term management for optimal foot health.
Broken ankles need immediate treatment. If you are seeking treatment, contact Naim G. Shaheed, DPM from Ankle and Foot Centers of Georgia. Our doctor can provide the care you need to keep you pain-free and on your feet.
Broken Ankles
A broken ankle is experienced when a person fractures their tibia or fibula in the lower leg and ankle area. Both of these bones are attached at the bottom of the leg and combine to form what we know to be our ankle.
When a physician is referring to a break of the ankle, he or she is usually referring to a break in the area where the tibia and fibula are joined to create our ankle joint. Ankles are more prone to fractures because the ankle is an area that suffers a lot of pressure and stress. There are some obvious signs when a person experiences a fractured ankle, and the following symptoms may be present.
Symptoms of a Fractured Ankle
- Excessive pain when the area is touched or when any pressure is placed on the ankle
- Swelling around the area
- Bruising of the area
- Area appears to be deformed
If you suspect an ankle fracture, it is recommended to seek treatment as soon as possible. The sooner you have your podiatrist diagnose the fracture, the quicker you’ll be on the way towards recovery.
If you have any questions, please feel free to contact one of our offices located in Lithonia/Stonecrest and Emory/Midtown, GA . We offer the newest diagnostic and treatment technologies for all your foot care needs.